Large Practice
- Home
- Large Practice
Medicure Healthcare and large practices pursue similar aims
- Shared Goal: Medicure Healthcare and large practices both prioritize providing high-quality healthcare.
- Efficiency and Performance: Both entities aim to optimize operational efficiency and financial performance.
- Patient Focus: Both entities prioritize patient care and satisfaction.
- Regulatory Compliance: Adherence to industry regulations is a shared goal.
- Collaboration Benefits: Working together can enhance the overall quality and accessibility of healthcare services.
Faster cash receipts
Error-free billing & coding
Enhance patient satisfaction
Complete denial resolution
Adherence to regulations
Cost-effective solutions
Our medical billing services feature a strong and reliable billing infrastructure
Our robust billing infrastructure offers transparency, affordability, and flexibility, addressing the shortcomings of traditional billing processes.
Medicure Healthcare provides efficient billing services, backed by up-to-date denial management resources and experienced personnel, offering solutions and round-the-clock support.

8 vital KPIs to expedite return on investment
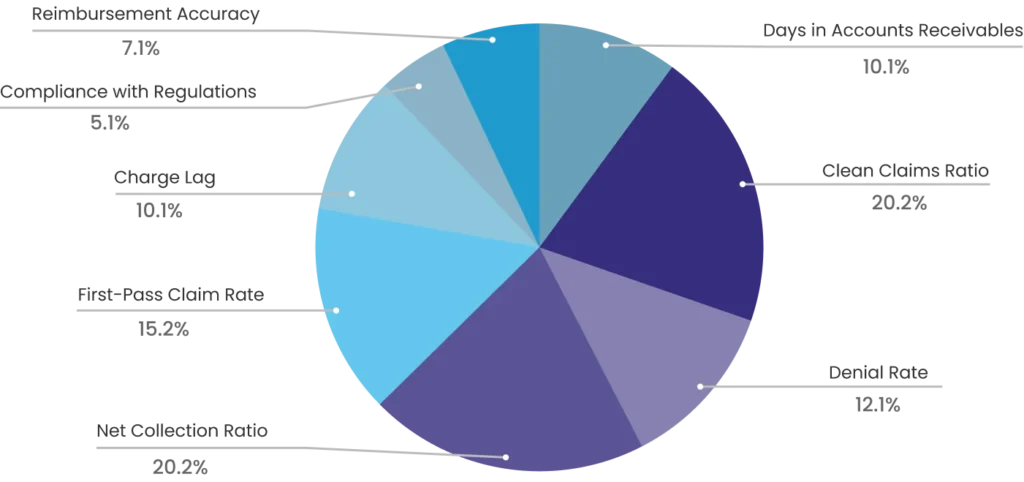
Elevate your billing, coding, and RCM performance with customized medical billing solutions
Medical billing solutions to optimize revenue cycle management for large practices
Eligibility check
Patient Registration
Claims Submission
Coding & Documentation
Denial Management
Payment posting
A/R Follow-up
Patient Billing
Education & Outreach
Our efficient processes expedite our ability to reach these objectives
24/7 Access to Technology and Infrastructure
Medicure Healthcare offers cutting-edge billing technology, coding tools, and infrastructure that enhance operational efficiency and provide personalized billing and RCM solutions for large practices. Outsourcing billing to us allows you to leverage these resources without the overhead of software or hardware costs.
Regular Auditing & Quality Control
We ensure regular internal audits to scan inaccuracies and point out areas for improvement in the billing processes. Not only that, we rectify the patterns and ensure quality control measures, such as double-checking claims and conducting reviews. This allows a reduction in revenue holes and inaccuracies.
Upfront Communication
Effective communication between insurers, administrative staff, and billing personnel is essential for building strong, lasting partnerships. It fosters trust and minimizes misunderstandings and errors.
Expertise & Specialization
Our team's experience and professionalism are key to reducing denials. By outsourcing billing to us, your large practice can access this expertise and ensure compliance with billing regulations.
Simplifying Complex Coding System (ICD-10, CPT, HCPCS)
We prioritize staying informed about the latest regulatory changes, coding guidelines, and insurance requirements. Our team of skilled coders, proficient in ICD-10, CPT, and HCPCS coding systems, ensures accurate coding and faster collections.

